Since when did my BMI determine my right to treatment?
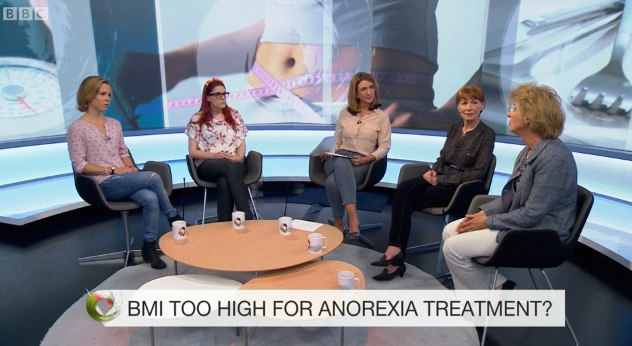
I was honoured to be invited onto the BBC 2 Victoria Derbyshire show to speak about a topic very close to my heart, and one which I am passionate about: Mental Health and access to treatment.
Recovery is a process that is long, and its journey cannot be completed alone. Treatment is an important step in anyones journey, whether that is recovering from depression, a broken leg or cancer.
Doctors, nurses, dieticians, psychiatrists…and many more, will all come into play.
Therapists and counsellors play a pinnacle role in helping recovery from many of the underlying psychological problems associated with eating disorders and mental health illness, and also help unite all members of the wider family together to optimise the recovery environment for the individual.
When recovery proves too hard, or the physical state of the individual poses serious risk to their health, and the wellbeing of the wider family, then inpatient treatments are also available….or not so it would seem.
With such fantastic services available the door to access them can be hard. Worse, can even promote deterioration rather than promote health.
On this episode of BBC 2 Vicotria Derbyshire show, I shared one of my experiences trying to access treatment as an adult (18+), and actually being denied help because my BMI was apparently not “low enough” although I was way below the average healthy weight, with difficulty breathing at night, and bed sores from protruding bones.
Eating Disorders are a mental health illness with physical symptoms, so when did BMI become an appropriate measure of my mental state and its manifesting behaviours?
As it stands, the very inaccurate form of measurement ‘Body Mass Index’ (BMI) is still used in the assessment criteria and access to treatments for many suffering with disordered eating.
Body Mass Index is a measure of standardised body weight that accounts for age, gender, height and weight. It is used to determine whether someone is healthy or unhealthy for their age and gender. However, it’s inaccuracies lie in the fact it has no reflection of where that weight is coming from (body fat/muscle mass), so many rugby players or bodybuilders are deemed ‘overweight’ by BMI although at peak physical fitness. This is important as it’s body fat that has the highest link with disease, such as diabetes and cardiovascular diseases, and not weight per-say.
When can using weight in the treatment of disordered eating be useful?
To fully heal something you need to understand it. Focusing on the weight restoration is the quick fix solution outlined by the medical model of recovery. Just like if you break an arm you wear a cast, or you have the flu so you rest in bed with antibiotics. If you look malnourished then it’s common sense to just re-feed them yes?
It is understandable, logical and fixable.
In mental health treatment there is so much grey area for what works best and for who and how long. It incorporates medical systems, family, friends, the society and individual environments to maintain and optimise health outcomes.
Do not get me wrong re-feeding is an important part of recovery. Low weight and starvation causes imbalances in hormones and brain functioning; further impacting impacts mood, thinking, anxiety levels etc…
It is necessary to correct these in order for therapy to be successful, and in some cases beginning therapy at a low weight will just have no use, because the individual will not be able to process the sessions or be fully present in them. BMI is often used as a measure to when a patient can begin gentle exercise without putting pressures on the heart, and damaging bone density.
The issue of weight in eating disorders
There are many different eating disorders, and the list is growing now, thought to coincide with the increase in social media diet trends such as “clean-eating”, “paleo”, “keto”, and the Westernised obsession with thinness, often associated with success and the beauty ideal.
Food is used as a form of communication, celebration, punishment and many other non-physiological uses that surpass the need to refuel, nourish and help our bodies perform.
The behaviours engaged in by disordered eaters (weight loss, exercise obsession; restriction etc…) are form of communication to the world that something is not right. It 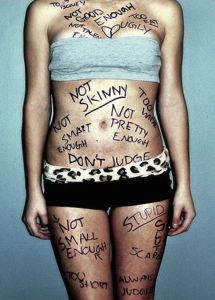 varies person to person why the the control of food and weight has manifested.
varies person to person why the the control of food and weight has manifested.
It can be a way to communicate feelings of self-doubt, self punishment, anxiety. Or to suppress difficult emotions or trauma that have left the individual feeling out of control.
It can take courage and bravery to step forward and admit there is a problem. The control and restriction is a blanket of comfort. Many fear losing it as it’s their way of getting through each day, and managing difficult thoughts and emotions.
Whilst weight loss is often achieved and maintained below the healthy level in anorexia, the diagnostic criteria varies hugely for various sub-types of anorexia, and is completely different for diagnosis of bulimia, binge eating disorder or orthorexia.
Each distinguishable by its behaviours and not the individuals weight.
They are all complex and multifaceted illness that cannot be constrained or measured by the weight or BMI of an individual.
Rather, a holistic approach needs to be given to the individual. Research points towards early intervention as giving the best prognosis, so it seems completely contradictory to leave it until he critical stages of physical and mental health to intervene.
A waste of money on the research if it’s not even going to be implemented in practice.
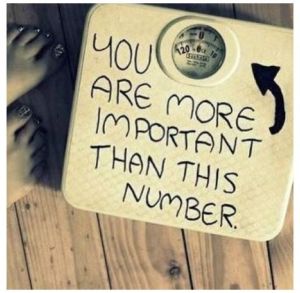
Your health should not, and is not, dependent on a number. Neither should your mental health be measured and confined to fit a stereotypical and superficial constraint.
When trying to rehabilitate someone who is so obsessed and controlled by numbers, that their whole world of self-worth revolves them, that they aren’t worthy of treatment simply reinforces everything they believe about themselves.
Whilst also demeaning the hard work it has taken for them to realise there is a problem that needs addressing.
Why rejection based on weight be so damaging for eating disorders
Rejection from treatment increases self doubt, feelings of unworthiness, and can lead to more extreme dieting and restriction techniques. You have reinforced their anorexia saying they’re too “big”, and ignored their cry for help for the world of pain the eating disorder is causing.
Behaviours can reach a point where they are so reliant on them it is a compulsive obsession, and the longer the person is left the more risk they are in for further health complications, and at worst, death.
Eating disorders have the highest mortality rate of any mental health illness and this is commonly due to suicide.
Furthermore, abandonment by services when a “goal weight” has been reached has equally poor outcomes for the patient. The surface problem has been mended but you’ve left the inside still broken.
For me, this just reflects a lack of training in the general practitioners and health care professionals in the area of mental health and treatment of eating disorders.
What’s it like to have anorexia and be a “normal weight”?
This is a picture of me in summer 2009, just after being discharged from my first inpatient unit where I’d received [very good] treatment [albeit not great therapy]  for 8 months.
for 8 months.
When I was discharged I was left without any help from CAMHS (child and adolescent mental health services) and although I look so happy and confident, on the inside I remember being so anxious, and had all the faulty thoughts of my anorexia whirling like a storm in my head that holiday.
I remember standing there hating every inch of my body in that photo. I was so unrestful, and unrelaxed on our lovely family holiday. I wanted to eat, to relax and enjoy myself but I just couldn’t hear my own thoughts in the whirlwind of my eating disorder.
The underlying psychological illness that remained was still destroying my life, and the lives of my family.
I was left vulnerable to relapse, with no understanding of how to cope and continue challenging my faulty thoughts and engrained coping mechanisms.
By the end of the summer I was back in another inpatient unit somewhere new. Somewhere far from home.
Having anorexia and having a normal body weight was hard work, and mentally tiring – no one realises you’re ill, no one thinks you need help, and you are more likely to be accused of attention seeking and not taken seriously.
It seemed so counterproductive for the NHS to spend SO much money on inpatient beds (we are talking 1000s of pounds) for them to touch on such a superficial part of recovery. The weight and food.
In Conclusion
The BMI debate continues…
Many are left denied treatment based on a number. But hopefully this post has opened your eyes to how unreliable that number is, and what a poor reflection it is of someones mental wellbeing.
Being denied access to treatment on the basis of BMI is a dangerous, and damaging, experience that can cause greater pain and suffering for all involved, as well as causing a greater expense to the NHS further down the line when more critical intervention is needed.
We need to deepen our understanding of mental health illnesses, and implement the research into medical practice that suggests early intervention has the best prognosis. This prevents individuals deteriorating to such as a critical stage, and can help save the health care system money in the long term.
BMI is a faulty key preventing many from opening the doors they need to health and freedom, and is an inaccurate portrayal of someones mental wellbeing.
I hope this has been insightful and thought provoking. Please do contact me or leave a comment if you have any more interest in this topic, or your own experiences to share. I am happy to say I am fully recovered and have been for many years now.
So have hope.

One Comment Add yours